Canadian researchers have proposed a method to detect COVID-19 infection rates in wastewater through sewer sensors.
The COVID-19 pandemic has presented a challenge to researchers because some of the spread of the virus has been from people that show no symptoms of the virus (1). Known as asymptomatic carriers, it is unknown how many cases of COVID-19 have been spread by asymptomatic versus patients with symptomatic COVID-19.
COVID-19 is typically detected by diagnostic tests, antibody tests, or COVID-19 management tests (2). However, people that are asymptomatic are not likely to get tested. As restrictions begin to ease, there is an increased risk that people with asymptomatic COVID-19 may spread COVID-19 unknowingly.
Detecting COVID-19 early
Early detection and treatment for COVID-19 could help to reduce the spread and damage done to at-risk populations. Methods for early discovery include detecting physical symptoms such as cough, fever, fatigue, nausea & vomiting, and appearance of the mucous membranes.
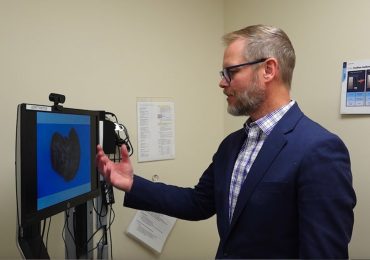
Most of the methods for early detection, however, require patients to travel to a testing site, further increasing their risk for spreading infection instead of socially distancing or staying at home. Researchers in Canada have proposed a unique early detection system that would utilize sewer sensors to identify COVID-19 hotspots (4). They published their results in the journal PLOS ONE.
Detecting COVID-19 in wastewater
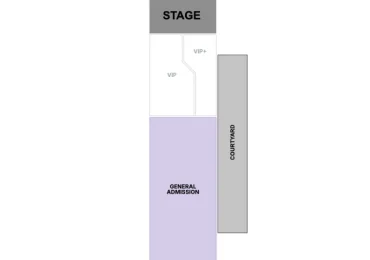
Researchers from the University of Toronto’s Rotman School of Management proposed using a sophisticated algorithm to calculate COVID-19 infection hotspots. The calculation would be based on data collected from sensors that are part of a Wastewater-Based Epidemiology (WBE) program.
Wastewater-Based Epidemiology is a new tool that can rapidly monitor the spread of diseases through the analysis of a population’s wastewater (5). Most people with COVID-19 excrete remnants of the SARS-Cov-2 virus in their waste, which ends up in the local wastewater system. Using advanced mathematical models, WBE data can be used to detect newly infected people or infection hot spots (4).
Identifying COVID-19 hotspots
To accurately trace hotspots, researchers identify the wastewater transport network from neighborhoods to wastewater treatment plants (WTP). Individual manholes are identified from which wastewater samples can be pulled for testing. If the samples test positive for SARS-Cov-2 virus remnants, researchers assume a neighborhood upstream from that sampling point has people with COVID-19, since it was detected in the wastewater. If the samples are negative, the neighborhood is negative.
Due to the size of cities and the number of potential sampling points, it would be impossible for researchers to sample and test each one. Using the mathematical algorithm, researchers can more accurately identify manholes and neighborhoods that are hotspots for COVID-19 infection. As part of the WBE, semi-permanent sensors would be placed in selected manholes. These sensors would be able to identify in real-time any ‘red-light’ COVID-19 infections in the wastewater.
Real-world testing
While in-manhole sensors have not yet been developed, the WBE method of sampling and testing wastewater has been trialed at several university dorms. For example, in the fall of 2020, the University of Arizona monitored and tested wastewater from manholes next to student dorms. When signs of COVID-19 infection were detected in the wastewater, all students in the dorm were tested. The student with COVID-19 was then isolated to ensure the health and safety of the remaining students (6).
Study authors say additional research is needed for a fast, inexpensive, and simple COVID-19 test for the wastewater samples. Also, in-manhole sensors need to be developed. Finally, research needs to be performed to determine how the wastewater systems themselves would affect the proposed detection and test methods proposed by the researchers (4).
In a press release, study author Professor Oded Berman said, It’s exciting to work on something that is very much needed and might have the potential to help people soon,” he said. “It’s very different from what I’ve done before.”
References:
- Dobrovolny HM. Modeling the role of asymptomatics in infection spread with application to SARS-CoV-2. Lo Iacono G, ed. PLOS ONE. 2020;15(8):e0236976. doi:10.1371/journal.pone.0236976
- Health C for D and R. In Vitro Diagnostics EUAs. FDA. Published May 24, 2021. Accessed June 7, 2021. https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/in-vitro-diagnostics-euas#individual-antigen
- Hashmi HAS, Asif HM. Early Detection and Assessment of Covid-19. Frontiers in Medicine. 2021;7. doi:10.3389/fmed.2020.00311
- Nourinejad M, Berman O, Larson RC. Placing sensors in sewer networks: A system to pinpoint new cases of coronavirus. Oliva G, ed. PLOS ONE. 2021;16(4):e0248893. doi:10.1371/journal.pone.0248893
- Sims N, Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: Monitoring infectious disease spread and resistance to the community level. Environment International. 2020;139:105689. doi:10.1016/j.envint.2020.105689
- Larson RC, Berman O, Nourinejad M. Sampling manholes to home in on SARS-CoV-2 infections. Adrish M, ed. PLOS ONE. 2021;15(10):e0240007. doi:10.1371/journal.pone.0240007
- Image by NickyPe from Pixabay